Call to action on ‘glaucoma ticking time bomb’
Campaign infographic
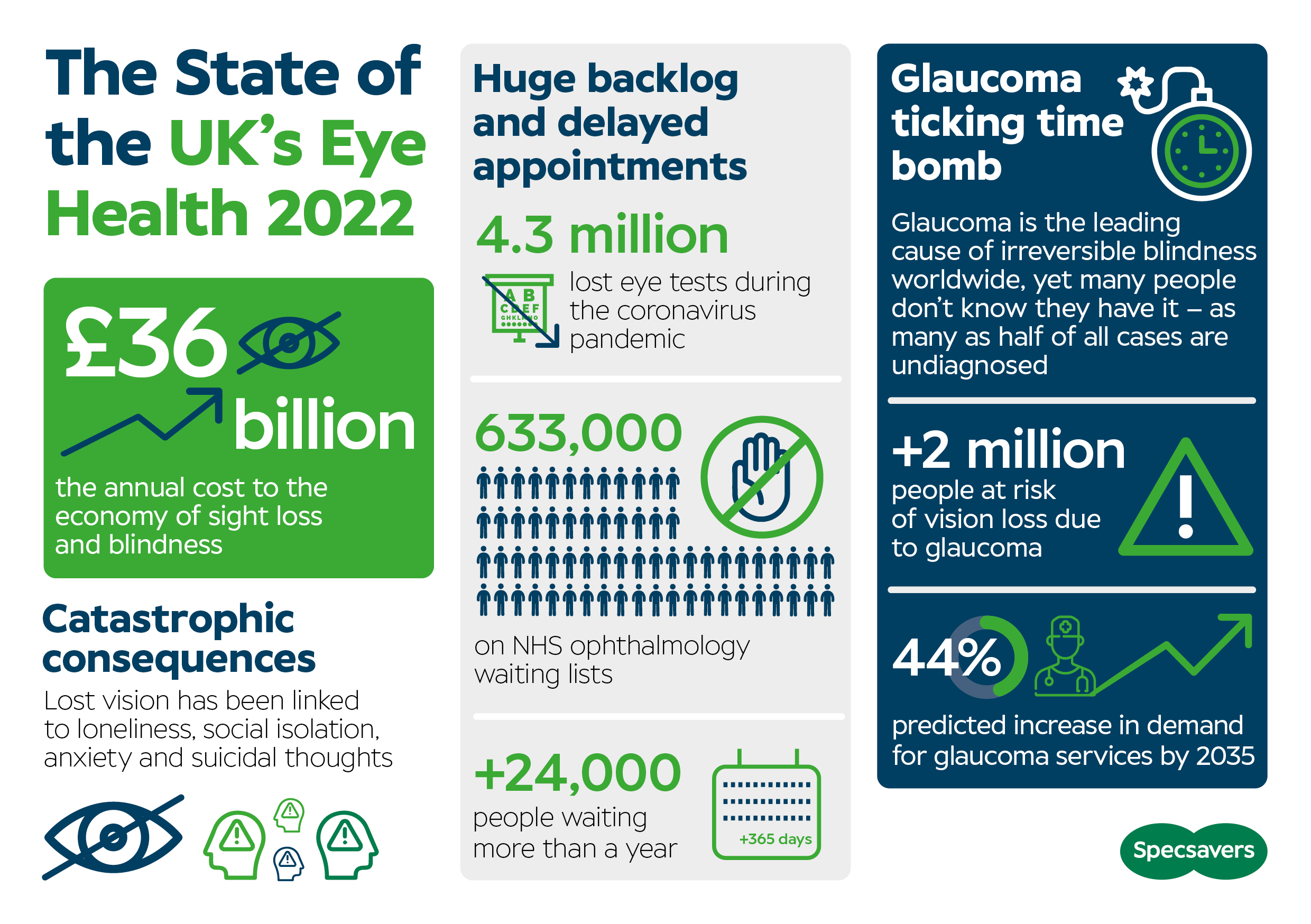
Ahead of World Sight Day on 13 October, Specsavers has released its State of the UK’s Eye Health 2022 report – highlighting ‘a glaucoma ticking time bomb’ in the wake of rising demand for services and the after-effects of the pandemic.
Launched today during a live digital event hosted by broadcaster, author and journalist, Dr Michael Mosley (pictured), the report is backed by Marsha De Cordova, MP for Battersea, and Lord Low of Dalston CBE, co-chair of the All Party Parliamentary Group on Eye Health and Visual Impairment.
Written by eye health experts, the report warns more than two million people with glaucoma and ocular hypertension are at risk of vision loss – yet there are long waiting lists for NHS ophthalmology appointments. Despite risk stratification, it’s said that new patients are waiting 18 months for an appointment in some areas.
The Royal College of Ophthalmologists predicts demand for glaucoma services will increase by 44 per cent by 2035. With the ageing population the situation will only get worse unless major changes are made.
The report claims that 633,000 people were waiting for NHS ophthalmology appointments in May 2022, and that more than a third of ophthalmology patients had not been seen within 18 weeks, the maximum waiting time set out in the NHS constitution. Further, 24,200 people has been waiting longer than a year.
In addition, parliamentarians warn of the huge economic cost of sight loss and blindness. The annual cost was estimated at £36bn in 2019. Due to the pandemic, this is expected to rise by £2.5bn between 2020 and 2024.
Total new registrations received by 13 charities managing the Sight Impairment Register for 19 Council areas in England and Scotland increased by 59 per cent in the year ending March 2022 compared to the previous year, and by 18 per cent compared to the year ending March 2020, pre pandemic.
Eye health experts say an enhanced role for community optometrists – working with ophthalmologists – is crucial. The assessment follows a joint vision statement from the College of Optometrists and the Royal College of Ophthalmologists setting out how primary and secondary care providers can work together to deliver high quality patient care. This is now underpinned by new guidance that maps clinical training to glaucoma patient pathways.

Report highlights opportunities for professional collaboration between optometry and ophthalmology
Professor Bernie Chang, president of the Royal College of Ophthalmologists, said: “This joint guidance empowers local optometrists with specified qualifications to manage patients in the appropriate glaucoma risk categories within their primary care settings. Only by increased working in multidisciplinary teams, with everyone working to the top of their licence and skill set, can we ensure patients with glaucoma are looked after in a timely manner in the right setting. This will reduce the risk of avoidable sight loss and protect our nation’s eye health.”
Professor Anthony King, consultant ophthalmologist and chair of Glaucoma UK, says the pandemic saw the eyecare sector re-evaluate how it functions, accelerating delivery of virtual clinics and prioritising high-risk patients using risk stratification tools.
“It also reviewed care pathways, shifting more care to community-led models where appropriate and enabling those at lower risk of sight loss to be monitored by qualified community-based health care professionals, particularly High Street optometrists,” said Professor King. “These actions undoubtedly helped those patients in the greatest need of care, but many more are still waiting to be seen.”
Writing in the report, Specsavers co-founder, Doug Perkins, said: “We have guidance from NICE and our professional bodies for standardised glaucoma care pathways, and this report highlights examples of community optometry and ophthalmology services collaborating effectively to meet patient need and save sight. More than ever, our leadership conversations need to be driven by data and evidence to scale these up at pace, drawing on the tools and expertise already in place in the community.”
The important role of dispensing opticians and contact lens opticians in triaging patients was highlighted during the launch event, along with the need for eyecare professionals to stop working ‘in silos’ and to foster a cohesive approach to tackling all the issues, from raising awareness of the help that local support and charitable organisations can provide, to the need for regular eye examinations and early diagnosis. Sharing data via clinical audit was also an area that needed to be pushed out within the eyecare sector.
Read the report here.