Focus on … DED management
Management and therapy
It is at this point that the patient may be referred back to the DO for advice, guidance and future management and it is important that the understanding of the subtype of DED and the correct management pathway is confirmed.
It is very safe to say that there is no single way to manage dry eye, just as the disease is multi factorial in its aetiology so is the pathway to the return to homeostasis and each patient may respond differently to different elements of therapy. It is also vital that the patient understands that there is no quick fix and therapy is an ongoing process.
We have already covered the classification differences and the prevalence of sub-categories. We have also noted that the vast majority of patients presenting with DED will have at least an element of the evaporative nature clinically apparent, so when it comes to putting a management package together for any patient the treatment should suit the needs.
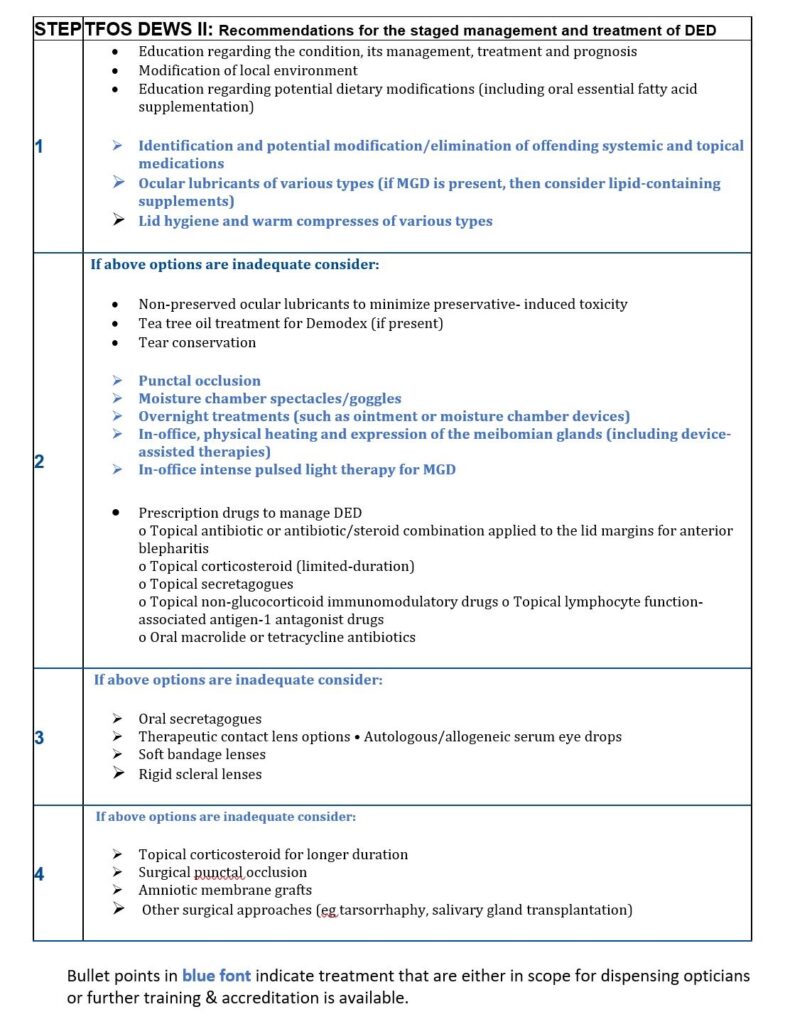
Figure 49 below lists the recommended staged management process for treating DED, the majority of patients we are likely to see will be covered in step one.
Some will move into step two, if the practice is set up for speciality dry eye management or have IP qualified optometrists then more patients managed in step two would be experienced by DOs, but from there steps three and four are moving into the realm of secondary care or specialist practice.
To remain within scope we will concentrate on step management.
Fig 49 Recommendations for the staged management and treatment of DED
Ocular lubricants
This is the most widely used area of management and also possibly the most mismanaged. Over the counter artificial tears do not target underlying pathophysiology. At the time of writing there were reported to be more than 100 examples of ocular lubricant drops, gels or ointments (preserved and non-preserved) on the market, but fewer than 10 per cent of these are designed for any element of EDE.
This vast array of products attempts to increase tear film volume, by targeting at least one layer of the tear film. They are safe but have some side effects, namely, transient visual disturbance, ocular discomfort and foreign body sensation. There are also variabilities in required doses and retention times. This is quite a rapidly expanding market and it is important to keep up to date with updates on what is available. As the product range is many and variable, detailed information on individual products should be sourced from manufacturers and attention given to not just the active ingredients but also their concentrations.
Aqueous supplementations feature a wide range of viscosity enhancing agents which aim to increase retention time on the ocular surface, the flip side of this, if viscosity is too high, is the blur effect and possible attraction of debris on the lids and lashes which may increase irritation, reduce tolerance and compliance. The DEWSII report reviews the wider range of these viscosity enhancers in detail11.
In practice many of the most popular products can be found with the inclusion of hydroxypropyl methylcellulose (HPMC), or hyaluronic acid (HA), in varying concentrations. HA acts in a non-Newtonian way, meaning viscosity decreases as shear forces, increase. For example, the effect of the blink makes the drop less viscous with the aim of minimising the blur effect which a more viscous liquid would create and a better balance of viscosity and elasticity can be created. HA is also known to bind to epithelial cells potentially giving it healing benefits.
Hydroxypropyl guar (HP Guar), is another constituent which exhibits these non-Newtonian properties through a pH dependant process. When released onto the eye the pH reduces and crosslinking between the HP Guar and other constituents creating a low viscosity gel which spreads easily over the ocular surface without the blur of a gel. This has been shown to increase mucin layer thickness, reduce inflammation and protect the ocular surface.
Lipid supplementations. As discussed earlier, ADDE represents only approximately 15 per cent of the dry eye population. This mismatch means that much of the treatment given for EDE or mixed dry eye is not getting to the root cause of the problem and probably not even managing the symptoms effectively. Consideration should be given to lipid-based supplements and lubricants for any patient with any form of MGD or EDE; these may come in the form of liposomal sprays or lubricant eye drops containing phospholipids and mineral oils to supplement the lipid layer and reduce the evaporative effect, leading to a more stable tear film and eventually a return to homeostasis.
These drops or sprays may contain mineral oils and/or phospholipids, fatty acids or triglycerides and are made as emulsions, allowing the oil and water to mix. They may be described as macro, nano or micro emulsions depending on the droplet size. Minimising the size of the droplet can optimise the delivery and effectiveness of the formulation.
It is important for anyone recommending ocular lubricants that the nature of the DED is understood in order to treat the primary cause of the disease and manage the long term and that the benefits of the therapy offered match this rather than being a short-term treatment.
A brief word about preservatives. Non-preserved treatments are often referred to as a first line approach due to the possibility of preservative reaction. Much of this concern dates back to challenges with treatments preserved with benzalkonium chloride (BAK) which can cause epithelial cell death and compromise tear film stability, however BAK is not a preservative used in the range of products we have available as lubricant eye drops. Instead, newer variant preservatives have been designed which have a lower impact on the ocular surface. So, although ideally a non-preserved drop may be a choice for a more advanced or severe case, the higher cost, greater difficulty in using, or availability may mean a preserved drop is the first choice for many patients. Note also that preservative free is a consideration recommended at stage two. (Fig49)
Lid hygiene and warm compresses
The final elements of stage one management options for the EDE/Mixed patient are those of lid hygiene and warm compresses.
Lid hygiene is often discussed for various conditions which relate to dry eye including blepharitis. A popular treatment has been bathing and wiping the lids with a solution of baby shampoo. You only have to look at what a detergent does to an oily layer to understand how this should not be suggested as a therapy for DED. This method of cleaning, although gentle and cost effective, has been shown to be ineffective and potentially worsen the condition by the breaking down of the mucins present. Given the wide range of proprietary single use lid scrubs, wipes and foams available these should be recommended instead.
Alongside lid hygiene, patients with MGD should also be guided in lid heat therapy and lid massage. Common advice of old would have been to warm the lids with a hot face cloth before gently massaging the lids with a rolling motion to loosen the aberrant meibum and free the meibomian gland openings. This outdated advice is not only likely to be unhygienic itself but also insufficient to heat the meibum through temperature or duration and is leading to poor compliance.
A temperature of over40°C is required for optimal warm compress treatment. It must also be kept in place for five minutes. Neither of these conditions are likely to be achieved with a heated face cloth, however several commercially available products are now available to make this an easy to follow process.
Gentle massaging of the lids following warm compress will promote expression of the material from the obstructed glands allowing the gland to function more normally, however, following heat care must be taken not to apply pressure to the eye itself by rubbing which could raise a risk of deformation of the cornea and visual blur. The patient should be carefully advised of the correct procedure for lid massage, by gently rolling the finger down the lid towards the lid margin, or massaging along the lid margin, all of course with clean hands.
It is likely that this procedure should be followed for between two to six weeks and may have to be ongoing, depending on severity.