What is glaucoma?
Everyone’s eyes are filled with fluid, known as aqueous humour. This fluid helps keep your eyeball in shape and circulates through a tiny meshwork round the edge of your iris. In some people the pressure of the fluid is raised and damages the optic nerve, which carries messages from your eye to your brain. In other people, although the pressure is not raised, there may be a weakness which causes similar nerve damage. In many people it can be a combination of nerve weakness and raised pressure which predisposes them to glaucoma.
How many people have glaucoma?
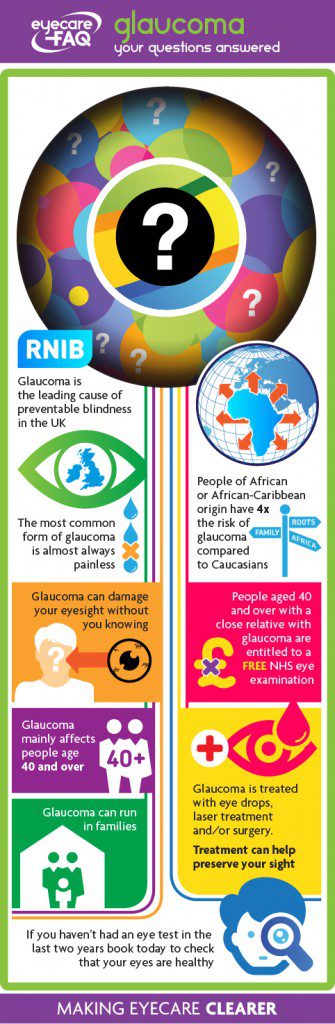
Glaucoma affects more than 700,000 people in England and Wales alone.
Who gets glaucoma?
It principally affects those age 40 and over: 2 per cent of people aged 40+ have glaucoma and this rises to almost 10 per cent of those over 75. People of African or African-Caribbean origin have about four times the risk compared to Caucasians.
Does glaucoma hurt?
In the UK, the most common form of glaucoma is almost always painless, which means that unless you have regular eye checks with an optometrist it can damage your eyesight without you realising. It is the leading cause of preventable blindness in the UK.
One of my parents has glaucoma. What does that mean for me?
Glaucoma can run in families: if you have a close relative with the condition you have four times the chance of developing it
If you have a close blood relative who has glaucoma – You are able to have a NHS funded eye test every year or at a recall period recommended by your optometrist.. It is important to ensure you are seen regularly at your opticians once you are aged 40+.
I’ve been told I have glaucoma. What now?
If you have been told that you have glaucoma you will need monitoring and treatment for the rest of your life to help protect your sight.
What is the main type of glaucoma?
Most of the time when we talk about glaucoma, we mean Primary Open Angle Glaucoma (POAG). This is painless and in the early stage you will have no warning signs. In POAG, the fluid in the eye can flow to the meshwork through which is should drain, but its flow is then restricted. The blockage happens slowly over many years, and the pressure in your eye increases gradually too.
What is ‘normal’ pressure?
NICE, the National Institute for Health and Clinical Excellence, has issued guidance that people with eye pressure of over 24 mmHg should be referred for further investigation. This is the case if the raised pressure is in one or both eyes.
What is ocular hypertension?
If you have raised pressure and no signs of damage to the nerves in the eye, this is called ‘ocular hypertension’. This could affect between 3 and 5 per cent of people aged 40+, and means that you may be at risk of glaucoma in the future. You will be asked to come back for regular checks and may be offered eye drops to protect your sight.
What is ‘low tension’ or ‘normal tension’ glaucoma?
A smaller number of people have a type of POAG where the pressure is within normal levels. This is known as Normal Tension Glaucoma. It may be due to poor blood circulation around the optic nerve. As with other types of glaucoma, treatment aims to lower the pressure in your eye to a level where the nerves do not suffer further damage.
My eye hurts. Is this likely to be glaucoma?
An uncommon type of glaucoma is acute glaucoma or angle closure glaucoma. This happens when the circulation of fluid round the eye is blocked suddenly. It can be caused by a narrow opening or ‘angle’ between the front of the iris and the drainage meshwork in the eye. It is sudden and painful and can cause permanent damage if untreated. If you experience a sudden painful eye, call NHS Direct for advice on 111.
What other types of glaucoma are there?
Glaucoma can be caused by other eye problems: this is known as secondary glaucoma. A very small number of babies are born with a problem that causes the pressure to rise in their eyes. This is known as developmental glaucoma.
Who is at risk of glaucoma?
For POAG, the most common type of glaucoma in the UK, there are several well known risk factors. You have a higher risk of the condition if:
- You are over 40. The risk increases as you age so glaucoma is present in five per cent of people over 65
- You are of African or African-Caribbean descent – the condition can develop at an earlier age and be more severe
- You have a close blood relative who has glaucoma – You are able to have a NHS funded eye test every year or at a recall period recommended by your optometrist.. It is important to ensure you are seen regularly at your opticians once you are aged 40+.
- You are very short sighted
- You have diabetes as this is believed to increase your risk of glaucoma
How is glaucoma detected?
Most people can’t feel or spot the early changes caused by glaucoma, so how can it be detected? Fortunately, these early changes can be spotted as part of a routine eye examination. Everyone should get their eyes checked at least every two years, and more often if advised. If you have a close family member with glaucoma, the International Glaucoma Association recommends that you are tested for glaucoma from the age of 35 onwards. If you are at higher risk of glaucoma because you are African Caribbean or if you have diabetes mention every time you have an eye test and ask to be checked for glaucoma, whatever your age.
What tests help the optometrist check me for glaucoma?
During the eye test the optometrist will carry out some tests to help them get a picture of your overall eye health. They will:
Look at the back of your eye with a light. In glaucoma the ‘optic nerve head’, where the optic nerve joins the eye, changes appearance, which can be seen using an ophthalmoscope
Measure the pressure in your eye – this can be done using an instrument that blows a puff of air on the eye or using a small probe that rests gently on the surface of your eye
Check your field of vision – you will be asked to put your chin on a rest and look at a screen where small spots of light will flash up one after another
If your eye pressure is raised your optometrist may invite you back for a further check to see if this is always the case.
My eye pressure is high. What happens now?
If the optometrist spots signs of glaucoma they will write a letter explaining this to your GP. Your GP will then pass these details on to the hospital eye department. You will be sent an appointment to see an ophthalmologist, a specialist eye doctor.
At the hospital you will have tests that are similar to those at the opticians, plus further assessments.
I’ve been referred to the hospital. How do they check for glaucoma?
NICE recommends that to diagnose glaucoma, the ophthalmologist should:
- Check the pressure in your eye using ‘Goldmann applanation tonometry’, where you put your chin on a rest, a blue light is shone on the eye and a small probe is rested gently on the eye surface. The ophthalmologist will use eye drops with this test. If you normally wear contact lenses, bring your glasses with you to the appointment as you will be advised not to put the lenses back in.
- Examine your eye with a special device which touches the surface of your eye gently to measure the thickness of the cornea, the clear front part of your eye.
- Assess the depth of the angle in front of your iris leading to the meshwork that the aqueous fluid should pass through.
- Check your field of vision. You will be asked to put your chin on a rest and look at a screen where small spots of light will flash up one after another.
- Use eye drops to get a good clear view of the back of the eye to see if the head of the optic nerve is showing any signs of change due to glaucoma. The drops used in this test can leave your vision blurred for a short while after the test. Do not attempt to drive yourself home afterwards.
What is the treatment for glaucoma?
Glaucoma can be treated and in most cases managed. There are various different types of treatment dependent on the type and severity of the glaucoma.
However, if your sight has been damaged there is not yet a treatment that can regain your lost vision. Treatment can only protect the vision that you have. The International Glaucoma Association estimate that around 95 per cent of those diagnosed early with glaucoma in the UK will retain useful sight for life. The main treatments for glaucoma are eye drops, laser treatment and drainage surgery.
How do eye drops help to treat glaucoma?
Eye drops help your eyes by opening up the drainage meshwork in your eye or reducing the amount of fluid produced: in this way the pressure in your eye goes down.
Eye drops help your eyes by opening up the drainage meshwork in your eye or reducing the amount of fluid produced: in this way the pressure in your eye goes down.
How does laser treatment help to treat glaucoma?
Laser treatment is now becoming increasingly common as a first line treatment option alongside the option of eyedrops. It works by increasing the drainage of fluid from the eye thereby reducing the pressure or by reducing the amount of fluid that the eye produces.
How does surgery help to treat glaucoma?
Drainage surgery, also known as trabeculectomy creates a channel that the fluid in the eye can drain out through. You may need to use eye drops too after surgery.
How long will I need to take eye drops for if I have glaucoma?
At the appointment you should have the chance to talk about your diagnosis, and ask about what might happen in the future. The eye specialist should explain that glaucoma is usually symptom less and you need to keep coming back to have it monitored. You will be told to persist with your treatment as it is needed to protect your sight. After your initial appointment, if you are prescribed eye drops you will be invited back within a few months to check that the drops are having the necessary effect. If everything progresses well you will continue to use your eye drops and have checks at regular intervals, every 6 months or annually depending on what your consultant advises. If you are given eye drops you will need to continue to use these for life unless the specialist changes your treatment or suggests laser treatment or surgery.
Where can I find out more about glaucoma?
If you are confused by any of the terms used during your appointment or want to find out more, the International Glaucoma Association has an excellent glossary on their website and can also answer questions through their Sightline, on 01233 648 164. www.glaucoma-association.com
What is the long term outlook now I have glaucoma?
Once you have glaucoma you will get your eyes checked at the hospital on a regular basis. The hospital specialist will let you know if the damage to your eyes is enough to cause problems with driving. The International Glaucoma Association offers a useful leaflet about driving when you have glaucoma.
I already have sight loss due to glaucoma.
If you already have sight loss due to glaucoma there are a number of ways to help you make the most of the vision that you do have. Ask at the hospital appointment to talk to a low vision specialist who can advise you on aids to help. A rehabilitation officer can advise and help you too.
How can I better care for someone with glaucoma?
If you care for someone with sight loss due to glaucoma, be aware that moving around is the area that they are most likely to have problems with. When crossing the road, they will need to make a point of turning their head and using their hearing to double check for cars.
Inserting eye drops can cause problems for older people and anyone with arthritic fingers. There are various eye drop dispensers available to make the process of inserting eye drops much easier. These are available through the RNIB shop: see contacts for details of ways to get in touch.
Updated 20 September 2023